Maxillary Ridge Augmentation With Fresh-Frozen Bone Allografts
Cintia Mussi Milani Contar, DDS, MS, João Rodrigo Sarot, DDS, MS, Jayme Bordini, Jr, DDS, PhD, Gustavo Holtz Galvão, DDS, Gastão Vale Nicolau, DDS, MS, and Maria Angela Naval Machado, DDS, PhD
Purpose: The present investigation clinically and histologically evaluated the use of fresh-frozen bone in the reconstruction of maxillary alveolar ridges to confirm the effective bone fill and support for the placement of dental implants.
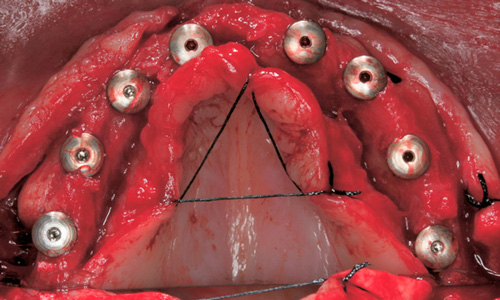
Patients and Methods: Fifteen patients who had atrophic maxillary ridge necessitating bone block grafts prior to implant placement were submitted to maxillary reconstructions performed with human block grafts of tibia fresh-frozen chips. Nine months later the re-entry procedures were carried out and at this time a bone core was removed from the grafts for histological analysis.
Results: Thirty-four blocks were placed, and the number of blocks each patient received ranged from 1 to 4. During the re-entry procedures, all of the grafts were found to be firm in consistency, well-incorporated, and vascularized. A total of 51 implants were placed over the grafts with a minimum of 40-Newton torque in all cases. None of the implants were lost. The follow-up period ranged from 24 to 35 months. The histological analysis revealed a living bone that showed features characteristic of mature and compact osseous tissue surrounded by marrow spaces.
Conclusion: Bone allografts can be successful as graft material for the treatment of maxillary ridge defects. If adequate surgical techniques are adopted, this type of bone graft can be safely used in regions of implant placement as a suitable alternative to autogenous grafts. © 2009 American Association of Oral and Maxillofacial Surgeons J Oral Maxillofac Surg 67:1280-1285, 2009
Bone grafting is essential for the repair of bone de-fects caused by tumors, trauma, loosening of pros-thetic joints, and prior dental implant placement in cases of alveolar ridge resorption.1-3 It is intended to stimulate bone healing and fill bone defects, with autologous bone grafting being the standard method of achieving these goals.4 Rapid incorporation and consolidation with a lack of immunologic consider-ations make bone harvested from the patient ideal.5 However, limited supply, donor site morbidity, in-creased blood loss, operative time, cost, and length of hospital stay are the main drawbacks of bone au-tografts.4-6
The use of bone allograft provides a reasonable alternative to meet the growing need for primary or supplementary graft material. The first bone allograft was performed in 1880 by a Scottish surgeon who successfully reconstructed the infected humerus of a 4-year-old boy with a graft obtained from the tibia of a child with rickets.7 Transplantation of large, fresh segments of long bone allografts continued and was expanded over the next 90 years.8 The establishment of the US Navy Tissue Bank in 1949 marked the emergence of the modern tissue bank.9 There is currently an in-creasing interest in bone allografts as a result of the development of bone banks in many countries.
Download
Maxillary Ridge Augmentation With Fresh-Frozen Bone Allografts
Surpreenda-se com o futuro!
WhatsApp
Facebook
Telegram
Email
LinkedIn
POSTAGENS RECENTES
Lançamento de Parceiros

Pensando em oferecer comodidade aos clientes o CENTRO DE DISTRIBUIÇÃO está localizado em uma região central da cidade de Curitiba.
Contato
E-mail: contato@systhex.com.br
SAC: +55 0800 600.6905
Tel/Fax: +55 41 3339.6905
WhatsApp: +55 41 9 8852-6995
Endereço: Al. Princesa Izabel, nº 1415
Bigorrilho – Curitiba – CEP 80730-080
2021 - Systhex Sistemas de Implantes Ósseo Integrado Ltda | Desenvolvido Nórtico Comunicação
